CSF – Critical Success Factors
Outcome measures in rehabilitation – the search for critical success factors
Several factors influence the course of convalescence during rehabilitation. Outcome measures and endpoints are often systematically associated with influences other than treatment, which may elicit different responses in different individuals. This leads to large variability and confounds the observed outcomes. In addition to the correct experimental design, influencing variables such as environmental and personal factors, temporal dynamics, initial values and, above all, the choice of method must be determined.
This also applies to new approaches such as artificial intelligence or machine learning, where performance depends equally on input variables and contextual factors: “Garbage In, Garbage Out”, whereby the data quality determines the quality of the results. Therefore, it is becoming increasingly important to find the right input and critical success factors to describe medical quality outcomes in rehabilitation.
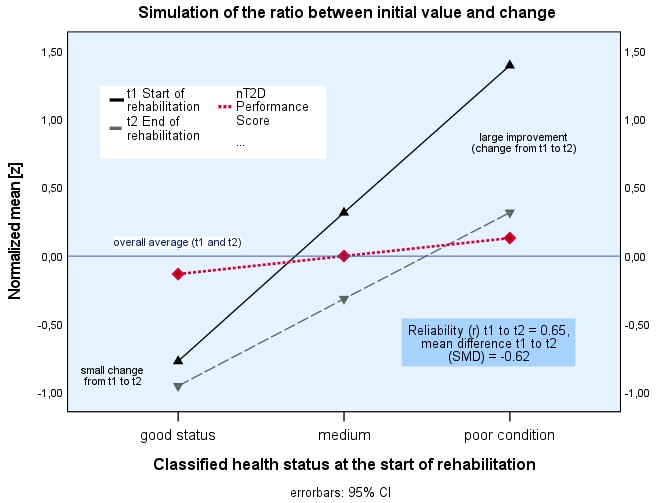
We analyse clinical outcomes for relevant moderating variables from rehabilitation practice and, last but not least, a suitable criterion that can be used for patient selection, the performance score classification (T2D). In rehabilitation, patient-reported outcome measures (PROMs) and clinician-reported outcome measures (CROMs) are used to assess a patient’s health status and recovery. Associations between CROMs and PROMs are low to moderate. Overall, rehabilitation in pre-post designs leads to an outcome with a large effect size. Women, the elderly, and patients with obesity and low physical activity often have poorer baseline scores (t1); therefore, they sometimes appear to respond better to the rehabilitation stay. However, differences between the start (t1) and end (t2) of rehabilitation alone do not reflect dynamic temporal changes over longer periods and often do not reflect clinical assessment practice, as changes between t1 and t2 often do not serve as valid indicators of what patients and clinicians report. For example, taking measurements of physical mobility can lead to ceiling effects. If a patient already has good mobility at the beginning of rehabilitation, no strong improvement is expected. Thus, these changes depend on the patient’s baseline status (Figure 1). The simple formula T2D = t2 + (t2 – t1) best reflects the performance and considers the individual state of health and changes due to rehabilitation treatments.
Our results and the use of the performance score represent a promising alternative approach. On the one hand, it takes into account a classification of the current health status and, on the other hand, the progression in the rehabilitation process (changes). We believe that the T2D concept is highly relevant for many studies and allows better clinical discrimination. Only a multidimensional collection of PROMs and CROMs – including the results of translational research on basic functional, biomolecular, and histological processes – offers an evidence-based and person-centered approach to improving health by providing medical rehabilitation for patients with functional deficits. To this end, T2D may be an appropriate external selection and validation criterion for new opportunities and applications to identify and evaluate critical success factors in rehabilitation.